According to a 2014 National Healthcare & RN Retention Report from NSI Nursing Solutions, economic improvement creates competition that impacts the attraction and retention of nursing and other hospital staff, largely due to the overall shortage of available, qualified personnel within the healthcare market. Consider the report’s conclusion:
The value hospitals place on their people will have a direct correlation to their commitment, confidence, and engagement. Enhancing culture and building programs to reinforce these values is critical to driving retention. Hospitals believe that retention is a “key strategic imperative,” yet are slow to translate this into a formal strategic plan.
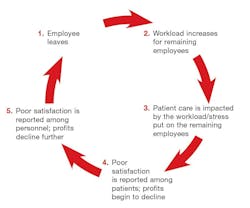
For healthcare settings, an employment attraction and retention strategy needs to be developed. Not only is it costly to replace an employee, but there is risk that the cycle will repeat and cause turnover to become the norm instead of the exception. The goal is to break this cycle and make attraction and retention the norm.
As healthcare designers, we have a very important role in assisting clients with staff attraction and retention. In addition to making staff members feel valued and appreciated, and providing them opportunities for professional growth, there are many opportunities to support the needs of employees, patients, residents, and visitors by improving the physical setting. Because of reimbursement, measuring the outcomes of healthcare design has been a hot button for many providers—but there has been a large focus on resident and patient satisfaction surveys and results, while further evaluation of staff satisfaction is often overlooked.
Collaborating with healthcare provider teams is essential to creating successful environments—and designers are a necessary contributor to the process! For example, there are several questions that directly relate to the physical environment in relationship to turnover rate:
- Are there spaces that support discussion and communication?
- Are walking distances supportive of the work that is required of an individual?
- Is the environment conducive to performing your job safely and efficiently?
Recently, I was re-reviewing a listing of concerns from a meeting agenda, and checking it against the current layouts that were being provided for the project. The staff member had written “FUNCTION, FUNCTION, FUNCTION”—meaning that not only do we need to make beautiful healthcare environments, but they also need to meet the operational needs for everyone working there.
Facilitating focus groups of all ages of staff can assist in better understanding their needs and concerns. Surveys are a good starting point, but interactive settings where it is safe to discuss and air out issues is the best way to support staff. Often we discuss completing a functional programming process prior to beginning the design of a healthcare environment. The information provides an opportunity to evaluate each operational and care activity so that it is appropriately supported by the design. This is similar to retention strategies; if you have a higher turnover rate, there is a need to address the “why” behind the issue.
PageBreakIn my recent visit to China to prepare for the opening of Cypress Gardens, a new resident-centered nursing home, a large portion of our discussion focused on training and re-training as a priority. In the beginning of the project, we evaluated a very detailed functional program that highlighted each operation and activity at the facility. We discussed training materials and the requirements needed for each function. For example, from a design perspective, discussing the entry sequence is important. It is necessary to consider the drop-off at the front of the community; the greeting/reception/concierge process for existing residents, prospective residents, and family members; the requirements for accessibility, storage, office space, and equipment; and most importantly, the first impression from aesthetic, branding, and welcoming perspectives.
Each of these design elements includes an operational component that requires training. We planned to implement a complete training program with mock-ups and role-play scenarios for Cypress Gardens. Taking a continual quality improvement approach, we begin by explaining the “why” aspects of a position, so that improvements are well-informed. Training is no longer a stagnant thing happening within a closed multipurpose room or bedside. Interactive opportunities can provide experiential training, supporting staff by fulfilling education and communication needs.
Communication is essential for successful healthcare projects. In the beginning of one design process, we were asked to come in and evaluate senior living designs that had been developed, but quickly realized that adequate input had not been gleaned from the existing residents, patients, and staff. The lack of communication created an atmosphere of distrust, conjecture, suspicion, and speculation about what was happening—spurring dissatisfaction. We were able to relieve the situation by holding focus groups for all of the stakeholders. Allowing everyone to feel heard is a critical factor. Satisfaction comes in following up with additional information, asking questions, and solving problems.
Regular communication that opens up channels from the top down as well as the bottom up can be a successful approach. Providing information in multiple ways is also important, considering the various employee ages. Apps are the latest wave for communicating in healthcare settings, but some staff may be uncomfortable with technology. Design can support communication by incorporating hubs and areas that are naturally conducive to interaction.
Providing unique opportunities for advancement also supports staff retention. This can be done through continuing education and also by allotting employees time to attend a class or participate in additional training. In China, staff housing is available and a meal during shifts is included as part of the compensation package. In the U.S., most of us are guilty of eating at our desks, but supporting communal meal settings allows for interaction and communication. Upon returning to China Senior Care’s office one afternoon, I found the entire staff participating in a stand-up exercise class together, building camaraderie and enhancing wellness. The director and administrator were side by side with IT, HR, communications, and administrative support staff. I tried thinking of ways that a similar concept could be brought back and implemented in my design firm. It would take a large cultural shift. Dance moves will take some time!
Jane Rohde, AIA, FIIDA, ASID, ACHA, AAHID, LEED AP, is the founding principal of JSR Associates, Inc., located in Ellicott City, Md. She champions a global cultural shift toward de-institutionalizing senior living and healthcare facilities through person-centered principles, research and advocacy, and design of the built environment. Clientele includes non-profit and for-profit developers, government agencies, senior living and health care providers, and design firms. Rohde speaks internationally on senior living, aging, healthcare, evidence-based design, and sustainability. For more information or comments, please contact her at [email protected].
About the Author

Jane Rohde
AIA, FIIDA, ASID, ACHA, CHID, LEED AP BD+C, GGA-EB
Jane Rohde, AIA, FIIDA, ASID, ACHA, CHID LEED AP BD+C & GGA – EB: Jane Rohde is the founding principal of JSR Associates Inc. in Catonsville, MD. JSR Associates Inc. celebrates 23 years of consulting services in 2019. Jane is the recipient of the 2015 Environments for Aging Changemaker Award and in 2018 she received the ASID Design for Humanity Award, was recognized as an Honorary Alumni of Clemson University’s Architecture + Health program, and has been honored as one of 10 notable Women in Design. For more information or comments, please contact Jane Rohde at [email protected] or “Chat with Jane” at www.jsrassociates.net.